Cyborg futures - the challenge of implanting and integrating artificial muscle
Also in “ Scientific meeting”



Discussion meeting organised by Professor Jonathan Rossiter, Dr Nazia Mehrban, Professor Martin Birchall, Dr Majid Taghavi, Professor Dario Farina, Dame Molly Stevens FRS FREng, and Dr Eleftheria Iliadou.
This meeting will be the first to address the scientific and social challenges of cyber-physical enhancement, robotic body restoration and implantable artificial muscles. The event brings together world-leading researchers and innovators to explore a cyborg future, with leading presentations and deep discussions in smart materials, implantable artificial muscles, neurointerfacing, soft robots, surgical implantation, biointerfaces, biomaterials, ethics and more.
Programme
The programme, including speaker biographies and abstracts, will be available soon. Please note the programme may be subject to change.
Poster session
There will be a poster session from 17:00 on Monday 9 June 2025. If you would like to present a poster, please submit your proposed title, abstract (up to 200 words), author list, and the name of the proposed presenter and institution no later than 11 May 2025. Submissions made after this date may not be included in the programme booklet.
Attending the event
This event is intended for researchers in relevant fields
- Free to attend
- Both virtual and in-person attendance is available. Advance registration is essential. Please follow the link to register
- Free lunch is available to all attendees on both days of the meeting
Enquiries: Scientific Programmes team.
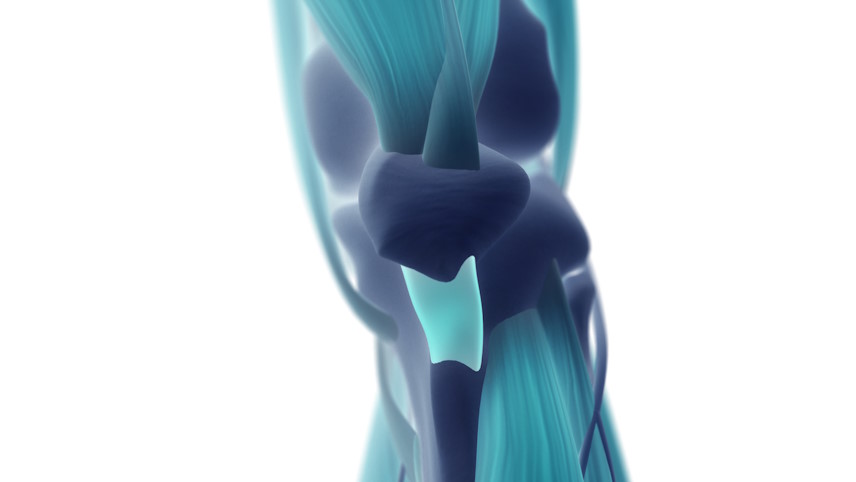
Image credit: ©️iStock/ChrisChrisW
Organisers
Schedule
Chair

Professor Wenhui Song
University College London, UK

Professor Wenhui Song
University College London, UK
Wenhui is a Professor of Biomaterials and Medical Engineering and Head of the UCL Centre for Biomaterials in Surgical Reconstruction and Regeneration at University College London's Division of Surgery and Interventional Science. Her research focuses on multi-responsive functional polymers, nanomaterials, nanocomposites, and biomanufacturing for biomedical applications. She leads a multidisciplinary team developing innovative biomaterials, including functional elastomers and nanocomposites for artificial organs and soft robotics, 3D responsive scaffolds for tissue regeneration and disease modelling, and nanofibre-guided iPSC-derived muscle and neuromuscular junction devices for drug discovery and hybrid biorobotics. Additionally, her work explores piezoelectric nanofibre-based biosensors for artificial muscle applications and AI-assisted artificial hearing systems.
| 09:00-09:05 |
Welcome by the Royal Society and lead organiser
|
|---|---|
| 09:05-09:15 |
Cyborg futures - engineering implantable artificial muscles
A future where people with disabilities and older people are restored to mobility and health through implantable muscles is very attractive, but faces huge challenges in technology, implantation, control and acceptance. Here we will review the latest progress in fundamental artificial muscle technologies for function restoration developed on the emPOWER project and at the University of Bristol's SoftLab. These include field-driven electrogels, liquid-metal self-oscillating fluid networks and functional hydrogels. 
Professor Jonathan RossiterUniversity of Bristol, UK 
Professor Jonathan RossiterUniversity of Bristol, UK Jonathan Rossiter is Professor of Robotics at the University of Bristol and Bristol Robotics Laboratory, and Royal Academy of Engineering Chair in Emerging Technologies. He is innovator of smart materials and soft robotics and leads the emPOWER EPSRC Programme Grant on Implantable Artificial Muscles and the VIVO Hub for Enhanced Independent Living. |
| 09:15-09:45 |
Developing a sensory representation of an extra robotic body part
Effective motor control depends on somatosensory feedback, yet artificial limbs are typically thought to lack this essential input. We explored whether the physical interaction of a wearable robotic device with the body could generate usable, natural sensory signals—sufficient to support a distinct neural and perceptual representation. Using the Third Thumb, a robotic augmentation of the hand, we compared natural tactile feedback with state-of-the-art artificial sensory systems. In material discrimination tasks, participants performed as well (or even better) with natural feedback, indicating it can be intuitive and functionally rich. To assess neural integration, we used fMRI to examine somatosensory cortex (S1) activity. Even with limited experience, the brain organised the Thumb’s tactile input in a topographic map and distinct from the palm. After a week of coordinated use, this representation became more finger-like, paralleling increased reports of embodiment. These findings suggest natural, physically mediated signals can foster the emergence of a sensory representation for robotic body parts—supporting their functional and experiential integration. 
Professor Tamar MakinUniversity of Cambridge, UK 
Professor Tamar MakinUniversity of Cambridge, UK Tamar Makin is a Professor of Cognitive Neuroscience at the MRC Cognition and Brain Sciences Unit at Cambridge University and the leader of the Plasticity Lab (www.plasticity-lab.com). Her main interest is understanding how our body representation changes in the brain (brain plasticity). Her primary model for this work is studying hand function and dysfunction, with a focus on how we could use technology to increase hand functionality in able and disabled individuals at all ages. |
| 09:45-10:15 |
From heart pump to face reconstruction: success and challenges in soft actuator implants
Whenever something moves in the human body, our muscles do the work. However, while today it part of everyday clinical practice to replace joints and bones with artificial parts, reconstruction medicine still has great difficulties finding a suitable replacement for damaged or destroyed muscles. There is one muscle in particular whose function is vital and is the subject of several studies, but without convincing results: the heart. Other muscles of the body actually share mechanical similarities with the heart, including the urinal sphincter muscle, which, if damaged, can cause urinary incontinence. Facial muscles also share such similarities and must be replaced after an accident or injury. Although these muscles do not play a vital role in the body, they remain extremely important for patients' quality of life, for example a well-functioning sphincter muscle is critical in order to avoid unpleasant side effects such as needing to wear diapers. The parallels between muscle types could allow the development of universal electroactive multifunctional actuators. Within the Centre for Artificial Muscles (CAM), EPFL, in cooperation with its partners in heart surgery, face reconstruction and urology - University of Bern and Reconstructive Medicine - University of Zürich, aims to become the world's leading reference for the development and clinical transfer of a brand new technological approach for artificial muscles in the human body. The proposed keynote intends to show some examples realised in this new centre. 
Dr Yves PerriardÉcole Polytechnique Fédérale de Lausanne, Switzerland 
Dr Yves PerriardÉcole Polytechnique Fédérale de Lausanne, Switzerland Yves Perriard obtained his Master in Microengineering from EPFL in 1989 and his PhD from the Electrical Department in 1992. He became cofounder of the company Micro-Beam SA and had the lead of the company until 1998 doing special electrical drives. In 1999 he joined EPFL as Senior Lecturer and in 2003 was appointed Titular Professor and leader of the Integrated Actuators Laboratory. In 2009 he was also appointed Vice-Director of the Microengineering Institute EPFL Neuchâtel. Senior member IEEE and Members EPE, he was also vice-president of the EPE (European Power Electronics) society board in Brussels. Yves Perriard is interested in innovating, analysing and creating new actuators associated with their electronic devices. The multi-disciplinary work of his research makes him strongly in contact with industries in Switzerland and abroad. Yves Perriard has published over 450 papers, 9 patents and is co-author of two books. He is associate editor of several journals. Teacher at the Bachelor and Master level, he has twice received the best teacher award of the Engineering Faculty in 2005 and 2007. More information can be found on the Integrated Actuators Laboratory website (http://lai.epfl.ch). In 2018, he launched a brand new centre at EPFL on artificial muscles thanks to a donation of the Werner Siemens Foundation. |
| 10:15-10:45 |
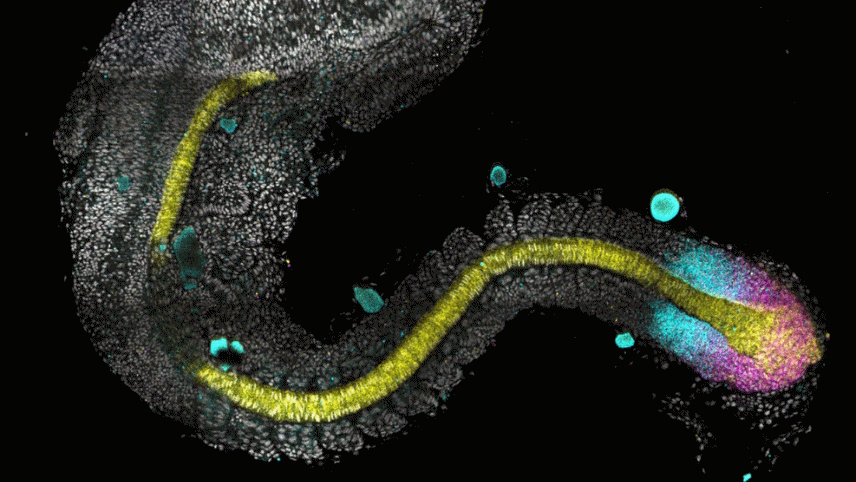
Advancing Biohybrid Robotics with Living Muscle
While synthetic actuators have enabled impressive robotic capabilities, they still fall short in replicating the adaptability, compliance, and energy efficiency of biological muscle. Biohybrid Robotics (BHR), which merges living tissues with artificial structures, offers a fundamentally different approach—one that reconstructs biological functions to both advance robotics and deepen our understanding of life. In this talk, I will introduce our recent advances in biohybrid muscle actuators using cultured skeletal muscle tissues. We have developed a range of architectures—including ring-shaped actuators, sushi-roll–style bundled constructs (MuMuTAs), and other multi-muscle configurations—that are optimized for different robotic functions such as walking, grasping, or slithering. These living actuators demonstrate high contractile force, modularity, and responsiveness to electrical stimulation, enabling novel types of soft robotic motion. Importantly, BHR is not merely a tool for engineering new machines; it is also a constructive approach to understanding biological mechanisms, such as coordination, force generation, and adaptability. By reconstituting these capabilities in engineered systems, we can explore principles that underlie neuromuscular control and tissue dynamics. The potential applications of biohybrid actuators are wide-ranging, from medical devices and drug testing platforms to environmental sensing and even cultured meat production. These possibilities position BHR as a key platform for shaping a cyborg future—one where biological and artificial systems merge in robotics, medicine, and beyond. 
Professor Shoji TakeuchiUniversity of Tokyo, Japan 
Professor Shoji TakeuchiUniversity of Tokyo, Japan Shoji Takeuchi received BE, ME, and DEng degrees in mechanical engineering from the University of Tokyo, Japan in 1995, 1997, and 2000, respectively. He is currently a Professor in the Department of Mechano-Informatics, Graduate School of Information Science and Technology, University of Tokyo. He has authored more than 250 peer-reviewed publications and filed over 140 patents. He has been recognised with numerous honours, including Young Scientists' Prize, the Commendation for Science and Technology by the Minister of Education, Culture, Sports, Science and Technology in 2008, the JSPS prize from Japan Society for the Promotion of Science in 2010, ACS Analytical Chemistry Young Innovator Awards in 2015, and UNESCO Netexplo Award Winner 2019. JSME Micro-Nano Science & Technology Achievement Award in 2022. His current research interests include cultivated meat, 3D tissue fabrication, bioMEMS, implantable devices, artificial lipid bilayer systems, and biohybrid machines. |
| 10:45-11:15 |
Break
|
| 11:15-11:45 |
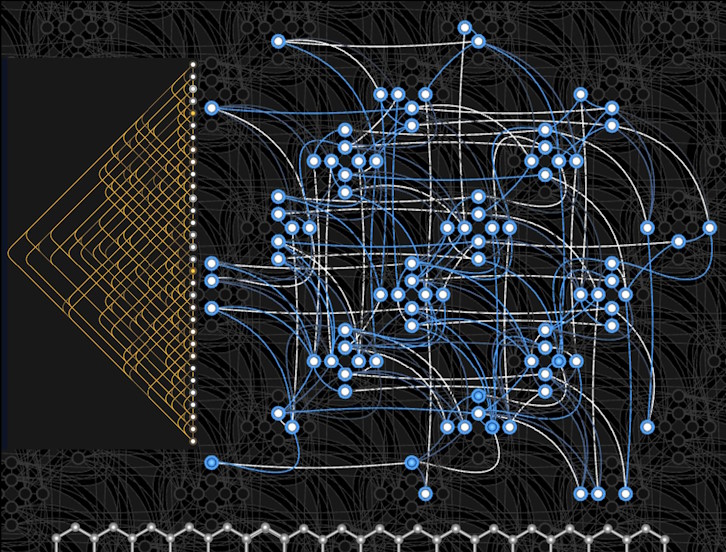
Soft microfabricated electrodes: expanding possibilities in neuroprosthetics and neural research (online)
Soft microfabricated electrodes are unlocking new possibilities in neural engineering by providing adaptable, biocompatible interfaces that seamlessly integrate with biological tissues. This talk explores recent advancements in these electrodes, focusing on two key applications: auditory prostheses and brain organoid research. In auditory systems, soft, multichannel implants are especially suited for conforming to the complex, curved surface of the cochlear nucleus, enabling precise simulation for patients who are not candidates for traditional cochlear implants. In brain organoid research, innovative electrode designs such as stretchable MEAs and the self-actuating "e-Flower" electrode provide high-resolution recordings of neural activity, even under mechanical strain. These applications highlight the transformative potential of soft electrodes to bridge the gap between engineered devices and complex neural systems, advancing both clinical therapies and fundamental neuroscience. 
Stéphanie LacourÉcole Polytechnique Fédérale de Lausanne, Switzerland 
Stéphanie LacourÉcole Polytechnique Fédérale de Lausanne, Switzerland Stéphanie P Lacour is full professor at the School of Engineer at the École Polytechnique Fédérale de Lausanne. She received her PhD in Electrical Engineering from the INSA de Lyon, France, and completed postdoctoral research at Princeton University (USA) and the University of Cambridge (UK). She joined EPFL in 2011. She is founding director of EPFL Neuro X institute - an interschool department focused on interdisciplinary and translational neuro-research located at EPFL-associated campus - Campus Biotech in Geneva. Since January 2025, she is EPFL Vice-President for support for strategic initiatives. |
| 11:45-12:30 |
Panel discussion
Mr Martin GarradUniversity of Bristol, UK Mr Martin GarradUniversity of Bristol, UK |
Chair

Dr Majid Taghavi
Imperial College London, UK

Dr Majid Taghavi
Imperial College London, UK
Majid Taghavi is an Associate Professor at Queen Mary University of London and a Research Fellow at Imperial College London, where he leads an interdisciplinary research group focused on Soft Robotics Transducers. He has also worked at SoftLab at the University of Bristol, UK, and the Italian Institute of Technology. Majid's goal is to pioneer the next generation of artificial muscles with enhanced functionalities, ultimately leading to the development of monolithic soft robots for healthcare applications. He has pioneered several artificial muscles, variable stiffness, and self-powered sensing technologies.
| 13:30-13:45 |
Separation of Neural Drives to Muscles from Transferred Polyfunctional Nerves Using Implanted Micro-Electrode Arrays

Professor Dario FarinaImperial College London, UK 
Professor Dario FarinaImperial College London, UK Dario Farina is Full Professor and Chair in Neurorehabilitation Engineering at the Department of Bioengineering of Imperial College London, UK. At Imperial College, he is also Director of the Imperial-Meta Wearable Neural Interfaces Research Centre. He has previously been Full Professor at Aalborg University, Aalborg, Denmark, (until 2010) and at the University Medical Center Göttingen, Georg-August University, Germany, where he founded and directed the Department of Neurorehabilitation Systems (2010-2016). Among other awards, he holds a Honorary Doctorate degree in Medicine from Aalborg University, Denmark, and has been the recipient of the IEEE Engineering in Medicine and Biology Society (EMBS) Early Career Achievement Award, the Royal Society Wolfson Research Merit Award, the IEEE EMBS Technical Achievement Award. His research focuses on biomedical signal processing, neurorehabilitation technology, and neural control of movement. Professor Farina has been the President of the International Society of Electrophysiology and Kinesiology (ISEK) (2012-2014) and is currently the Editor-in-Chief of the official Journal of this Society, the Journal of Electromyography and Kinesiology, and an Editor for many other international Journals, including Science Advances and IEEE Transactions on Biomedical Engineering. He has been elected Fellow IEEE, AIMBE, ISEK, EAMBES, AAIA, Sigma Xi. |
|---|---|
| 13:45-14:15 |
Interfaces with the peripheral nervous system: a possible route to the direct control of artificial muscles and the delivery of sensory feedback
Neural interfaces are most common in the CNS and have been used successfully to record and decode kinetic and kinematic movement intention at the macro scale for the control of upper-limb prostheses or robotic devices. However, the PNS offers micro scale access to the efferent and afferent pathways that innervate groups of muscles or sometimes single muscles, thus providing possible control inputs at the single muscle level. This talk will cover extra-neural and intra-neural PNS electrode designs, signal processing algorithms for decoding efferent information, stimulation approaches for somatosensory feedback, and the use of animal and human models for interface design and development. The goal is to show how PNS interfaces can provide muscle-specific efferent and afferent interfacing using technologies that are minimally invasive. 
Dr Ben MetcalfeUniversity of Bath 
Dr Ben MetcalfeUniversity of Bath Ben is a biomedical engineer with a focus on the development of healthcare technologies for human rehabilitation and enhancement. One recent example is the EarSwitch – a novel ear based assistive technology designed to enable those with diseases such as Motor Neurone Disease to communicate. He has a particular interest in peripheral nerve interfaces and has developed implants to restore control of the urinary bladder after spinal cord injury and to provide sensory feedback in upper limb protheses. In 2023 he co-founded the Bath Institute for the Augmented Human to advocate for the holistic design of neurotechnology taking into consideration the technological, regulatory, societal, and ethical implications. He has advised UK Government and the Ministry of Defence on the risks and opportunities associated with human augmentation and recently co-launched the OECD policy toolkit on neurotechnologies as the UK representative. |
| 14:15-14:45 |
Incorporating artificial muscles into devices and testbeds
My research is focused on device-enabled approaches to assist or augment dynamic tissue through active assistance and delivery of biological therapy. This talk will focus on representative implantable devices that we have worked on, each addressing an identified shortcoming of existing technologies. I will also discuss high fidelity organosynthetic testbeds incorporating artificial muscles designed to validate and interrogate device performance before advancing to in vivo studies. 
Professor Ellen RocheMassachusetts Institute of Technology, USA 
Professor Ellen RocheMassachusetts Institute of Technology, USA Ellen Roche is a Professor at the Institute for Medical Engineering and Science and the Department of Mechanical Engineering at the Massachusetts Institute of Technology. She directs the Therapeutic Technology Design and Development Lab. She completed her PhD at Harvard University School of Engineering and Applied Sciences. Her research focuses on applying innovative technologies to the development of cardiac devices. Her research includes development of novel devices to repair or augment cardiac function using disruptive approaches such as soft robotics, combination of mechanical actuation with delivery of cell therapy, and use of light activated biodegradable adhesives. Dr. Roche was employed in the medical device industry for over five years as a research and development engineer and employs her understanding of the medical device industry and the regulatory pathways to medical device commercialization in her academic research. She is an author on over 100 conference/journal papers. She is the recipient of multiple awards including the Fulbright International Science and Technology Award, the Wellcome Trust Seed Award in Science, a National Science Foundation CAREER Award, an NIH Trailblazer Award, a Charles H. Hood Award for Excellence in Child Health Research, the Harold E. Edgerton Award for Outstanding Faculty Achievement and the Presidential Early Career Award for Scientists and Engineers. |
| 14:45-15:15 |
Interfacing with the spinal cord: A pathway for restoring mobility after paralysis
Neural conditions such as spinal cord injury often result in the disruption of functions below the level of injury, including the loss of the ability to stand and walk. Neuroprosthetic approaches focused on activating peripheral nerves and muscles for restoring standing after paralysis have been successful; however, their use for restoring walking has been met with various challenges. These include the need for widespread implantation of electrodes and the control of numerous muscles that exhibit varying contractile and fatigue profiles. To address these challenges, we developed micro-implants that directly activate locomotor-related networks in the lumbar region of the spinal cord through intraspinal microstimulation (ISMS). With ISMS were are able to generate graded single joint movements and multi-joint synergies resulting in walking distances upwards of 1km in pre-clinical models. Our focus now is on developing translational versions of the spinal micro-implants and testing them in a pre-clinical model with spine and spinal cord dimensions and morphologies similar to those in humans. 
Professor Vivian Mushahwar FAIMBE FCAHSUniversity of Alberta, Canada 
Professor Vivian Mushahwar FAIMBE FCAHSUniversity of Alberta, Canada Dr Vivian K Mushahwar is a Professor of Medicine at the University of Alberta and Canada Research Chair (Tier 1) in Functional Restoration. She is also the Director of the Institute for Smart Augmentative and Restorative Technologies and Health Innovations (iSMART) and its business arm, Smart Technology (ST) Innovations. She is a Fellow of the American Institute for Medical and Biological Engineering and a Fellow of the Canadian Academy of Health Sciences. Her work focuses on developing intelligent wearable and implantable neuromodulation devices that restore mobility and prevent secondary complications. She also focuses on developing activity-based therapy rehabilitation interventions that are both efficacious and cost-saving. She initiated the development of micro-implants for stimulating the spinal cord to restore standing and walking after complete spinal cord injury, and demonstrated the benefits of simultaneous arm and leg cycling for improving walking capacity after incomplete spinal cord injury. She and her group invented the wearable garments, Smart-e-Pants and the SOCC, for preventing pressure injuries and deep vein thrombosis, respectively. She holds funding from numerous agencies including the Canadian Institutes of Health Research, New Frontiers in Research Fund, Brain Canada Foundation, and the US Department of Defense. |
| 15:15-15:45 |
Break
|
| 15:45-16:15 |
Muscles to embody uncertainty, optimally interact with the environment and extract information from it
In this talk, I will present how humans control their muscles to interact optimally with their environment and how implementing these principles can create versatile artificial muscle systems. Human muscles function as soft actuators with tunable spring-like properties, allowing for adaptive energy exchange, maximal sensory extraction, and compensation for stable, unstable, or uncertain dynamics. By modelling and implementing these adaptive mechanisms, we have developed robotic systems that advance flexible industrial automation, teleoperation, and intuitive, efficient human-robot interaction. 
Professor Etienne BurdetUniversity College London, UK 
Professor Etienne BurdetUniversity College London, UK Dr Etienne Burdet (https://www.imperial.ac.uk/human-robotics/) is Professor and Chair of Human Robotics at the Imperial College of Science, Technology and Medicine in the UK. He is also a visiting Professor at University College London. He holds an MSc in Mathematics (1990), an MSc in Physics (1991), and PhD in Robotics (1996), all from ETH-Zurich. He was a postdoctoral fellow with TE Milner from McGill University, Canada, JE Colgate from Northwester University, USA and Mitsuo Kawato of ATR in Japan. Professor Burdet's group uses an integrative approach of neuroscience and robotics to: i) investigate human sensorimotor control, and ii) design efficient interfaces for daily living technology and neurorehabilitation, which are tested in human experiments and commercialised. |
| 16:15-17:00 |
Panel discussion

Professor Marcus DrakeImperial College London 
Professor Marcus DrakeImperial College London Marcus Drake is Professor of Neurological Urology at Imperial College London, and Honorary Consultant Urologist at Charing Cross Hospital. He is also Honorary Professor of Physiological Urology at the University of Bristol. He undertook his medical training at the Universities of Cambridge and Oxford and was awarded his research Doctorate Thesis by the University of Oxford. His clinical interests in Urology are Urodynamics, Neuro-urology, LUTS and Nocturia. He is Chief Investigator of UK National Institute of Health Research grants in Male LUTS (HTAs UPSTREAM & TRIUMPH). He is co-CI of an NIH RO1 grant in Physiology (PDE5 effects on voiding). He is co-CI for minimally invasive surgery of the prostate (HTA PREMISE). He is an investigator on the UK EPSRC emPOWER study. He was CI of the MeNiMS study of nocturia in MS, Nocturia (RfPB PLANET), catheter design (RfPB Flume), recurrent stress incontinence (HTA PURSUIT), UTI diagnostics (i4i QUICK), BESIDE and NEPTUNE2. He was a co-investigator for MASTER, FUTURE, PRIMUS and CADET. His total cumulative career grant awards are £33M, of which £10M are as CI. He is a Trustee of the International Continence Society. He is member of NICE panels (recurrent UTIs and Male LUTS guideline groups, Intermittent Catheters late stage assessment). He was Chairman of the International Continence Society’s Standardisation Steering Committee, and board member of the European School of Urology and the European Society of Female and Functional Urology. He was a member of the European Association of Urology Guidelines committees for male LUTS and Female Incontinence. He has published major books, including the 4th Edition of “Abrams’ Urodynamics” and “Medicine in a Day” volumes 1 and 2. |
| 17:00-18:15 |
Poster session
|
Chair

Dr Nazia Mehrban
University of Bath, UK

Dr Nazia Mehrban
University of Bath, UK
Nazia Mehrban is Assistant Professor of Biotechnology at the University of Bath, UK. She received her PhD in ligament engineering from the University of Birmingham and has held post-doctoral appointments at University of Bristol and University College London with a visiting scholar position at University of Pittsburgh. Her interdisciplinary group works at the interface between biology, chemistry, and engineering focusing on fundamental underpinning work towards designing, manufacturing, and characterising bespoke biomaterials for unmet clinical needs. Her research crosses the boundary between natural and synthetic materials and uses a bottom-up design approach for the creation of novel materials. The innovative and bespoke ‘smart’ materials her group manufactures are chemically and physically tuneable allowing control of cellular behaviour towards various applications including tissue repair & regeneration, extracellular matrix reconstruction and integrative materials for implantable devices.
| 09:00-09:15 |
Designing biomaterials for regenerative medicine and soft robotics
This talk will provide an overview of our recent developments in bioinspired materials for applications in regenerative medicine with focus on establishing translational pipelines to bring our innovations to the clinic. Our group has developed fabrication methods to engineer complex 3D architectures that mimic anisotropic and multiscale tissue structures and generate spatially arranged bioinstructive biochemical cues. I will discuss recent advances in our tunable nanoneedle arrays for multiplexed intracellular biosensing at sub-cellular resolution and modulation of biological processes. We are developing creative solutions for targeted and controlled delivery using soft robotics and nanotherapeutics with unique bioinspired characteristics that respond to external stimuli to release a payload. Our design approach keeps state-of-the-art fabrication approaches while keeping in mind versatility and scalability to maximise the application potential. Finally, I will explore how these versatile technologies can be applied to transformative biomedical innovations and will discuss our efforts in establishing effective translational pipelines to drive our innovations to clinical application while actively engaging in efforts towards the democratisation of healthcare. Professor Dame Molly Stevens DBE FRS FREngUniversity of Oxford Professor Dame Molly Stevens DBE FRS FREngUniversity of Oxford Professor Dame Molly Stevens DBE FREng FRS is John Black Professor of Bionanoscience at the University of Oxford and also holds part-time professorships at Imperial College London and the Karolinska Institute. Professor Stevens’ multidisciplinary research balances the investigation of fundamental science with the development of technology to address some of the major healthcare challenges. She is a serial entrepreneur and the founder of several companies in the diagnostics, advanced therapeutics and regenerative medicine space. Her work has been instrumental in elucidating the bio-material interfaces. She has created a broad portfolio of designer biomaterials for applications in disease diagnostics and regenerative medicine. Her substantial body of work influences research groups around the world (>450 publications, h-index 123, >58k citations, Clarivate Analytics Highly Cited Researcher). Professor Stevens holds numerous leadership positions including Deputy Director of the Kavli Institute for Nanoscience Discovery and the UK Quantum Biomedical Sensing Research Hub, and Scientist Trustee of the National Gallery. She is Fellow of the Royal Society and the Royal Academy of Engineering (UK), Foreign Member of the National Academy of Engineering (USA), International Honorary Member of the American Academy of Arts and Sciences, and she has been recognised with over 30 international awards including the 2023 Novo Nordisk Prize. |
|---|---|
| 09:15-09:45 |
Biologic interactions of biosynthetic and biologic scaffolds and their effect on the constructive tissue remodelling (online)
The purpose of the talk is to provide an overview on how polymeric biomaterials, and particularly their degradations products, elicit differential responses by the immune cells at the biomaterial-tissue interface. Focusing on the biosynthetic surgical mesh composed of poly (4-hydroxybutyrate) (P4HB), a biomaterial widely used in the biomedical field for hernia repair applications, which has been associated with improved long-term remodelling response and decreased surgical site infection in pre-clinical and clinical studies. In our research, we have identified that 4-hydroxybutyrate (4HB), the main degradation product of P4HB and a short chain fatty acid (SCFA), endogenously secreted in the body, promotes a pro-remodelling, regulatory phenotype of macrophages, which partially contribute to the promotion of site appropriate tissue remodelling. Moreover, through our research it was found that 4HB increased the expression of antimicrobial peptides (AMP) in these macrophages. These studies provided insights on the associated molecular mechanism. It was identified that the mechanisms of AMP secretion are independent of a direct HDAC inhibitory activity, commonly associated with SCFA. Instead, it involves the transcriptional activation of cathelicidin LL-37 through MAP-kinase and NF-KB pathways. Key proteins identified in the transcriptional activation process were GPR109a, JNK, P38, NF-KB, and AP-1. The results of this work expand the understanding of the biologic activity of 4HB in immune system cells and demonstrate its potential to promote a constructive tissue remodelling effect for regenerative medicine applications. 
Professor Catalina Pineda MolinaUniversity of Pittsburgh, USA 
Professor Catalina Pineda MolinaUniversity of Pittsburgh, USA Dr Catalina Pineda Molina is a Research Assistant Professor at the Department of Surgery, working with Dr Stephen Badylak and Dr George Hussey at the McGowan Institute for Regenerative Medicine a the University of Pittsburgh. Prior to joining the University of Pittsburgh, she was was an Assistant Professor and Head of the Biomedical Engineering Program at Universidad CES, in Medellín, Colombia. In 2014, she received a Fulbright Scholarship to pursue her PhD in Bioengineering. Dr Pineda Molina's research interests are focused on tissue engineering and regenerative medicine applications, particularly developing and evaluating naturally derived biomaterials for the promotion of appropriate constructive tissue remodelling. In particular, she is interested in understanding the molecular mechanisms associated to host-biomaterial interactions and how these can be modulated through molecular bioactive markers, thus advancing in biomaterials science and the immunobiology associated to biomaterials. |
| 09:45-10:15 |
Forward Engineering of Multi-cellular Living Biological Machines (online)
The integration of living cells with 3D printed soft scaffolds can enable the realization of multi-cellular machines for a range of applications in engineering and medicine. We will review our group’s efforts and present recent results towards developing such centimeter scale biological machines that are actuated by skeletal muscles cells. These machines are controlled via electrical or optogenetic signals and demonstrate improved healing after a damage when exercised via optical stimulation. We have developed approaches for uni- and bidirectional movement and steering, and most recently are also working to integrate neural control in these biological machines. Using stem cells, a fibrin matrix, and 3D printed molds, we are able to form functional in vitro neural tissue mimic of different shapes, which can eventually be integrated in the walking machines. As these cellular machines increase in capabilities, exhibit emergent behavior, and potentially reveal the ability for self-assembly and self-repair, important questions can also arise about the ethical implications for this direction of research, which are very important to consider and address. These cellular systems present many opportunities in the next decade and beyond with potential applications in drug delivery, power generation, and other biomimetic systems. 
Professor Rashid BashirUniversity of Illinois Urbana-Champaign 
Professor Rashid BashirUniversity of Illinois Urbana-Champaign Rashid Bashir is Professor of Bioengineering, the Grainger Distinguished Chair in Engineering, and is currently the Dean of Grainger College of Engineering at the University of Illinois at Urbana-Champaign. He is an internationally renowned scholar in micro-fluidics, nanotechnology and 3D bio-fabrication. He has authored or co-authored over 320 journal papers and has been granted over 65 patents. He was on the founding team of the Carle Illinois College of Medicine, the Chan Zuckerberg Biohub Chicago. He is a member of the US National Academy of Inventors, the US National Academy of Medicine, and the American Academy of Arts and Sciences in 2024. |
| 10:15-10:45 |
Advancing the biofabrication of tissue building blocks
The seamless integration of biological and engineered components is essential for ensuring the functionality of artificial muscles. Engineered tissues hold great promised in facilitating the integration. Functional tissue building blocks, in particular, will allow the introduction of multiple functionalities into engineered tissues, further enhancing the integration of both biological and engineering components. Our research focuses on developing innovative biofabrication strategies to create functional tissue building blocks and exploring their potential to support the functionality of engineered tissues. In this presentation, I will present our work on microfluidic platforms for generating microvessel templates that guide a vascular integration within engineered tissues both in vitro and in vivo. Additionally, I will discuss how we leverage 3D printing, combined with magnetic control to fabricate thin-layered bioscaffolds and how these bioscaffolds facilitate the creation of 3D vascular networks and 3D biohybrid actuators. Furthermore, I will talk about the generation of magnetically responsive, cell-laden microgels with smart assembly and motion abilities and discuss their potential for dynamic, minimally invasive tissue delivery and interfacing. We believe these biofabricated building blocks provide promising strategies in supporting the implantation, (neuro)vascular integration, and muscular control capabilities of engineered tissues, and will contributed to the development of functional systems for enhanced muscular restoration. 
Dr Ruoxiao XieUniversity of Liverpool, UK 
Dr Ruoxiao XieUniversity of Liverpool, UK Dr Ruoxiao Xie is a Lecturer in Bioengineering within the School of Engineering at the University of Liverpool. She received her PhD from Tsinghua University in 2020. From 2020 to 2024, she worked as a postdoctoral researcher in Professor Dame Molly Stevens' group in the Department of Materials at Imperial College London. Her research group at the University of Liverpool focuses on developing engineered tissues and organ/organoid-on-a-chip platforms for applications in disease modelling, drug screening, and tissue regeneration. To achieve these goals, her team is also developing innovative biomaterials, biofabrication strategies and bioreactors to enhance tissue patterning and maturation, thus improving the functionality of engineered tissues and organ/organoid-on-a-chip platforms. |
| 10:45-11:15 |
Break
|
| 11:15-11:45 |
Cyber-Physical Enhancement of Therapeutic Cells and Tissues for the Clinic
Regenerative medicine principles are based on the ability of cells to regenerate and grow tissues in vitro and in vivo. Engineering provides the platforms and tools which enable the control and manufacture of cells used for clinical therapy and regenerative organ models. The interaction of biological and physical factors play a key role in providing the stem cell niche which is capable of rebuilding tissue complexity both in vitro and in vivo. One aspect of this is how to design platforms which can remotely control and integrate cells as a therapeutic; which can be used routinely within a hospital environment. Exogenous cell delivery or endogenous recruitment provide stem cell sources which require instructive delivery systems. We have developed multiple remote control platforms using magnetic nanotechnology approaches which can be aligned with advanced cell-based therapies. The challenge lies in engineering mechanical control solutions for stem cells which have clinical relevance. We are currently translating these approaches to the clinic. 
Professor Alicia El Haj FREngUniversity of Birmingham, UK 
Professor Alicia El Haj FREngUniversity of Birmingham, UK Professor Alicia El Haj is a leading UK figure in Bioengineering and Regenerative Medicine and has been involved in bringing together interdisciplinary groups within biomedicine, physical sciences and engineering to develop innovative new cell based therapies to the clinic. She has published over a 300 publications in novel enabling technologies such as novel cell and tissue engineering approaches, bioreactors technology, biomaterials and new imaging systems for regenerative medicine with funding from EPSRC, MRC, BBSRC, AR UK Innovate and EU FP in the UK. She is a co-Director of a CDT programme in Regen Med, and a UKRMP Hub in Engineering the Stem cell niche. ISTM has been progressing cell therapies into routine clinical use in orthopaedics for the past ten years working with consultant orthopaedic surgeons. She is also a Director of a spin out company, MICA Biosystems Ltd involved in translating her patents into clinical use. Professor El Haj was awarded a Royal Society Merit Award in 2014 and in March 2015, was awarded the MRC Suffrage Award for her role in leading women in STEM. |
| 11:45-12:30 |
Panel discussion

Dr Nazia MehrbanUniversity of Bath, UK 
Dr Nazia MehrbanUniversity of Bath, UK Nazia Mehrban is Assistant Professor of Biotechnology at the University of Bath, UK. She received her PhD in ligament engineering from the University of Birmingham and has held post-doctoral appointments at University of Bristol and University College London with a visiting scholar position at University of Pittsburgh. Her interdisciplinary group works at the interface between biology, chemistry, and engineering focusing on fundamental underpinning work towards designing, manufacturing, and characterising bespoke biomaterials for unmet clinical needs. Her research crosses the boundary between natural and synthetic materials and uses a bottom-up design approach for the creation of novel materials. The innovative and bespoke ‘smart’ materials her group manufactures are chemically and physically tuneable allowing control of cellular behaviour towards various applications including tissue repair & regeneration, extracellular matrix reconstruction and integrative materials for implantable devices. |
Chair

Dr Eleftheria Iliadou
University of Athens, Greece

Dr Eleftheria Iliadou
University of Athens, Greece
Dr Eleftheria Iliadou is an otorhinolaryngologist with clinical expertise and academic focus in audiology, neurotology, voice and swallowing disorders. Her research spans hearing aid counselling and usage optimisation, voice pathology, and the effects of noise and music exposure, with numerous publications in respected international journals. She has been a member of the London Hampstead Ethics Committee and maintains a strong presence in both national and international clinical research networks, participating in multidisciplinary collaborations across Europe. She is currently based in Greece, working at the 1st University Department of Otolaryngology and Head and Neck Surgery of the National and Kapodistrian University of Athens. Recently, she was appointed Associate Professor of Otolaryngology at the University of Peloponnese, highlighting her growing influence in clinical research and education.
| 13:30-13:45 |
Labs, animals and people: negotiating the road to implantable robots

Professor Martin Birchall FMedSciUniversity College London, UK 
Professor Martin Birchall FMedSciUniversity College London, UK Martin is a professor of laryngology at UCL and a consultant in ENT surgery at the Royal National Ear, Nose and Throat and Eastman Dental Hospital. He is a highly ranked academic otolaryngologist as measured by the impact of his research, teaching and papers. A specialist in disorders of voice, swallowing and breathing, he has pioneered the use of transplantation, tissue engineering and soft robots in surgery. Clinically, he has a particular interest in voice and swallowing, as well as the interface between upper GI medicine and laryngology. He treats patients with vocal cord weakness ('palsy') and pioneered new means of restoring function for them using the drive from unaffected nerves (laryngeal reinnervation). In interventional clinic, run with top speech and language therapists, he uses advanced technology, including transnasal oesophagoscopy, awake laser procedures and transcutaneous vocal cord injection, to treat throat and voice problems. He has a special interest in throat problems affecting persons with hypermobility disorders, including EDS. He has a large research network concentrating on the use of innovative technology to manage disorders of the head and neck, especially the use of biomaterials, cells, and soft robots. With Prof Elliott at Great Ormond St and others, he co-led the team which delivered the world’s first tissue engineered implants (tracheal) to a series of children between 2010 and 2014. In 2010, he was also part of the team which performed the world's second (and first functionally reinnervated) laryngeal transplant at UC Davis, California. He was Morgan Stanley Briton of the Year (Science and Technology), 2008, and is a frequent guest speaker at major international conferences. He has published in the Lancet, Nature and the BMJ. With Prof Sandhu and Prof Howard (Imperial College), he founded the British Laryngological Association in 2011, and helps run successful bi-annual conferences 'Cutting Edge Laryngology' and Soft Robotics in Healthcare (‘SoRo’). He was the first otolaryngologist to be elected to the Academy of Medical Sciences in 2010 and was awarded NIHR Senior Investigator status in 2012 and renewed in 2020. He is Trustee of both the National Association of Laryngectomee Clubs and the Throat Cancer Foundation. He is passionate about involving patients and publics in medical science, including the present innovative arts-science initiative “A Sound Voice”. He presently has a particular interest in how we may include access to clinical trials for all parts of society, overcoming barriers of race, ethnicity, language, gender identity and economic deprivation. He has long supported students from communities with less tradition of careers in science and medicine (“STEM” subjects), on to success in University applications and beyond. He has five children and is a keen road and gravel cyclist and an enthusiastic follower of Liverpool Football Club. |
|---|---|
| 13:45-14:15 |
Implants for the gastrointestinal tract. Towards resilient and responsive medical devices
The development of next-generation medical devices demands systems that are not only intelligent and functional, but also resilient, adaptive, and seamlessly integrated with the human body. This talk presents a robotics-viewed roadmap toward such capabilities through three core technological strategies. In-the-body Residential Devices: We explore the concept of robotic implants designed for long-term in vivo presence, capable of delivering continuous therapy and monitoring. These systems must navigate biological complexity while maintaining mechanical and functional integrity over extended periods. Resilient Devices: A central challenge in implantable and wearable technology is fault tolerance. We introduce approaches to designing devices with passive resilience, mechanisms that enable function-preserving responses to structural damage or environmental variation without relying solely on active control systems. Bio-artificial Interfaces: Finally, we address the need for interfaces that are both tissue-responsive and energy-efficient. We present emerging bio-hybrid sensors and actuators that can communicate bidirectionally with biological systems, while operating within minimal power constraints. These themes point towards a new generation of bio-integrated devices that can survive, adapt, and interact more intelligently with the human body, opening new possibilities for chronic care, precision therapy, and biological augmentation. 
Dr Dana DamianUniversity of Sheffield, UK 
Dr Dana DamianUniversity of Sheffield, UK Dana D Damian is a Senior Lecturer (Associate Professor) in the School of Electrical and Electronic Engineering at the University of Sheffield. She received her PhD from the University of Zurich in 2012. She was a visiting scholar at Johns Hopkins University, Stanford University, and Carnegie Mellon University (2011/2013). She was a postdoctoral research fellow at Boston Children’s Hospital, Harvard Medical School before joining the University of Sheffield. She leads the Sheffield Biomedical Robotics Laboratory where her group’s mission is to develop bionic and implantable devices that show life-like behaviour and sustain operation for long-term therapies, and are minimally invasive, in order to advance surgical treatments and regenerative medicine. Her research has been supported by EPSRC, UKRI, MRC and SNSF, and highlighted on BBC, at House of Lords, etc. |
| 14:15-14:45 |
Title to be confirmed
Mr Paolo De CoppiGreat Ormond Street Hospital, UK Mr Paolo De CoppiGreat Ormond Street Hospital, UK |
| 14:45-15:15 |
Translating Cyborg Futures into Present Practice: Building regulatory and commercialisation strategies
Developing innovative ‘Cyborg’ medical technologies in the laboratory with the potential to act as artificial muscles is of itself highly complex. Successful progression of those inventions from the benchtop to eventual adoption into clinical practice requires multiple challenges to be overcome en route. A critical aspect is that neuro-integrated implantable devices are classified as presenting the highest level of safety risk in the risk spectrum of medical technologies. This talk will introduce the importance of early consideration of regulatory and commercialisation strategies in the journey of these medical technologies to market access. It will draw on practical examples from non-implantable neuro-tech therapies to highlight some of the regulatory challenges and how they can be overcome, such as through the application of key standards. Future regulatory frameworks may be viewed as irrelevant to those undertaking fundamental research, however research funders, such as the UK Research & Innovation (UKRI), are increasingly expecting ‘realisable’ outputs of research i.e. ones that have potential to be put into practice and deliver real-world impact. The purpose of this talk is to emphasise the interactions between regulatory and commercialisation strategies with the aim of de-risking health technology research. Through such early de-risking, the likelihood of research translating into realisable outputs to benefit the ‘health and wealth’ of the nation increases. 
Dr Avril McCarthySheffield Teaching Hospitals NHS Foundation Trust, UK 
Dr Avril McCarthySheffield Teaching Hospitals NHS Foundation Trust, UK Avril McCarthy is a Consultant Clinical Scientist in clinical engineering at Sheffield Teaching Hospitals NHS Foundation Trust. A Fellow of The Academy for Healthcare Science, she has an established NIHR and EPSRC research track record spanning orthopaedic, continence and rehabilitative technologies. She received her PhD from the Faculty of Engineering, University of Sheffield. Following a post-doc position within a pan-European project to design a meniscal knee implant, collaborating with leading orthopaedic, software, and virtual prototyping companies, she worked clinically in gait and movement analysis for the NHS working, before concentrating on medical device innovation; most recently a neuro-stimulation device clinical trial for stroke rehabilitation. Avril has been a long-standing member of the leadership team of NIHR Long Term Conditions HealthTech Research Centre – Devices for Dignity, now leading its ‘Pathways to Implementation and Impact’ Theme. In addition, Avril has been an active member of the UK’s National Institute for health and Care Excellence (NICE) Medical Technologies Advisory Committee since 2016. |
| 15:15-15:45 |
Break
|
| 15:45-16:15 |
Ethical empowerment? Ethical aspects of the design, development and deployment of implantable artificial muscles
According to the opening credits to the 1970s science fiction TV series, The Six Million Dollar Man, cyborg technologies promise to make us “better – stronger – faster”. Such technologies are, of course, no longer the preserve of science fiction, they are science fact. Developments like implantable artificial muscles (IAMs) certainly seem to promise much to, and for, patients – and potentially others. At the same time, however, there are various ethical issues to consider when designing, developing, and deploying IAMs. Based on a narrative review undertaken as part of the emPOWER project, this presentation outlines some of the key issues, which concern: (a) serving the public interest, which includes considerations of public support, access and distribution, as well as responsibility and accountability; (b) balancing benefits and harms to not only recipients of IAMs, but also others; and (c) respect for autonomy (or self-rule), including questions of consent and confidentiality. Although future research could usefully hear more from those involved in, or likely to be affected by the development of IAMs, there is, prima facie, an ethical case for their development. But, when seeking to deliver on their promise, we should also take care to avoid and address the possible, plausible, or probable perils they might also present. 
Professor Richard HuxtableUniversity of Bristol 
Professor Richard HuxtableUniversity of Bristol Richard Huxtable is Professor of Medical Ethics and Law, based in the Centre for Ethics in Medicine, in the Medical School at the University of Bristol. His research interests include surgical ethics, clinical ethics, and end-of-life ethics. He has undertaken research on surgical innovation, as part of Bristol’s NIHR Biomedical Research Centre, and on the development of artificial muscles, as part of the EPSRC emPOWER project. Richard serves, or has served, on numerous ethics committees and boards, including those of the BMA, RCGP, Institute of Medical Ethics, the UK Clinical Ethics Network, and the European Association of Centres of Medical Ethics. |
| 16:15-17:00 |
Panel discussion

Professor Andrew ConnUniversity of Bristol, UK 
Professor Andrew ConnUniversity of Bristol, UK Andrew Conn is an Associate Professor of Robotics at the University of Bristol, who obtained a PhD from the same institution in 2008. He leads a group of 7 researchers in the field of biorobotics with a focus on the integration of functional materials and physical intelligence into systems such as mobile robots, wearable technologies and implantable healthcare devices. This is driven by the potential for great improvements in human-robot interaction and robot mobility in unstructured environments. |
